Beta-blockers are associated with better long-term survival in patients with Tako- Tsubo syndrome
Angelo Silverioa, Guido Parodib, Fernando Scudieroc, Eduardo Bossoned, Marco Di Maioa, Olga Vrize,f, Michele Bellinog, Concetta Zitoh, Gennaro Provenzag, Ilaria Radanog, Cesare Baldig, Antonello D’Andreai, Giuseppina Novoj, Ciro Maurod, Fausto Rigok, Pasquale Innellil, Jorge Salerno-Uriartem, Matteo Camelin, Carmine Vecchionea,o, Francesco Antonini-Canterinp, Gennaro Galassoa, Rodolfo Citrog,o.
a Department of Medicine, Surgery and Dentistry, University of Salerno, Baronissi, Salerno, Italy
b Department of Cardiology, ASL4 Liguria, Lavagna, Italy
c Cardiology Unit, Health Authority Bergamo East, Italy
d Division of Cardiology, Antonio Cardarelli Hospital, Naples, Italy
e King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
f College of Medicine, Al Faisal University, Riyadh, Saudi Arabia
g Division of Cardiology, Cardiovascular and Thoracic Department, San Giovanni di Dio e Ruggi d’Aragona University Hospital, Salerno, Italy
h Department of Clinical and Experimental Medicine, Section of Cardiology, University of Messina, University Hospital “Policlinico G. Martino”, Messina, Italy
i Department of Cardiology and Intensive Coronary Unit, “Umberto I” Hospital, Nocera Inferiore (Salerno), Italy
j Biomedical Department of Internal Medicine and Medical Specialties, Cardiology Unit, University of Palermo, Palermo, Italy
k Cardiology Department, Ospedale dell’Angelo Mestre-Venice, Venice, Italy
l Department of Cardiovascular Imaging, San Carlo Hospital, Potenza, Italy
m University of Insubria, Varese, Italy
n Division of Cardiology, Department of Medical Biotechnologies, University of Siena, Siena, Italy
o Vascular Physiopathology Unit, IRCCS Neuromed, Pozzilli, Italy
p Cardiology Unit, High Specialization Rehabilitation Hospital Motta di Livenza, Motta di Livenza, Treviso, Italy
INTRODUCTION
Although Tako-Tsubo syndrome (TTS) is generally considered a benign disease, recent evidence from large-scale registries has demonstrated a substantial morbidity and mortality during follow-up.[1, 2]
Supraphysiological serum levels of catecholamines have been reported in TTS [3, 4, 5] and could influence patients’ clinical outcome not only during the hospitalization but also at long term. On this basis, the use of beta-blockers has been proposed to mitigate the sympathetic drive, blunt the effects of further catecholamines’ surge, and avoid their potentially detrimental effect after the acute phase.However, to date the long-term prognostic benefits of beta-blockers has not been proven in TTS.[6, 7]
The aim of the present study was to investigate the impact of beta-blockers therapy on long-term outcomes of patients with TTS by using the information prospectively collected in the Tako-Tsubo Italian Network Registry.
RESULTS
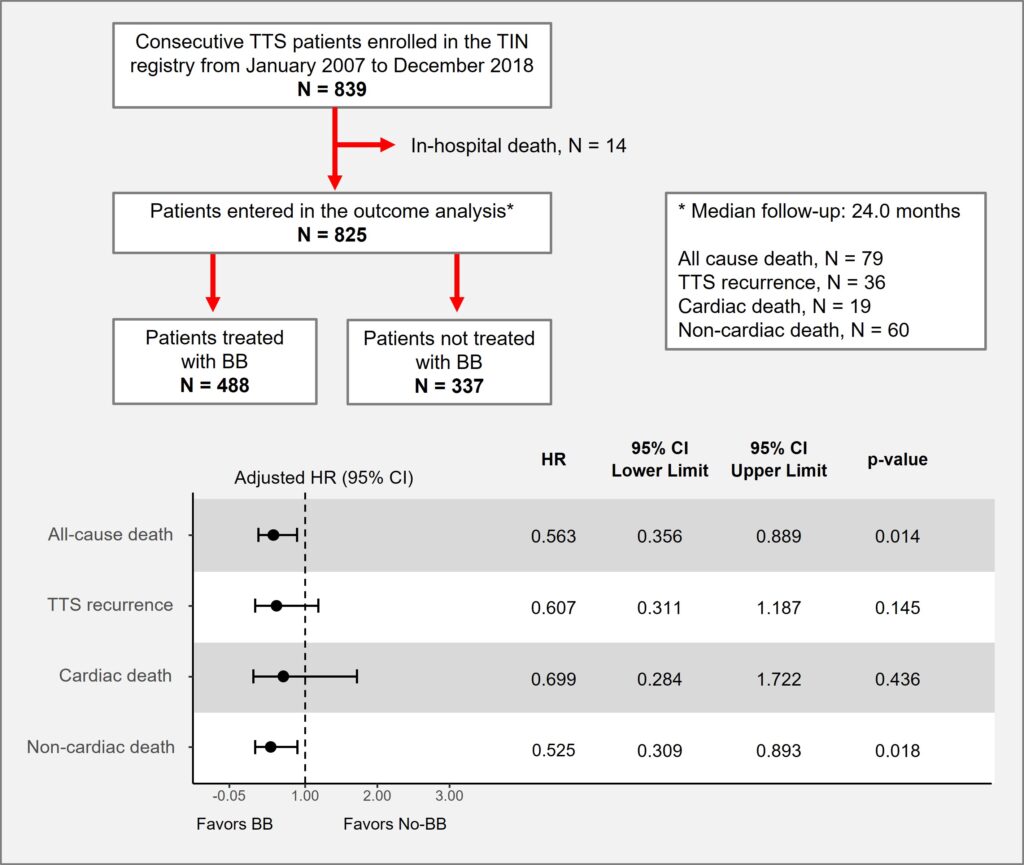
The study population included 825 patients with TTS diagnosis; 488 (59.2%) were discharged on beta-blockers, and 337 (40.8%) without beta-blockers. The median age was 72.0 (63.0-78.0) years and 91.9 % were females.
The prescription of beta-blockers at discharge was prevalent in patients with CAD (p=0.042) and in patients presenting with chest pain (p<0.001), while was lower in patients with COPD (p=0.029). No differences between groups were observed in terms of in-hospital complications.
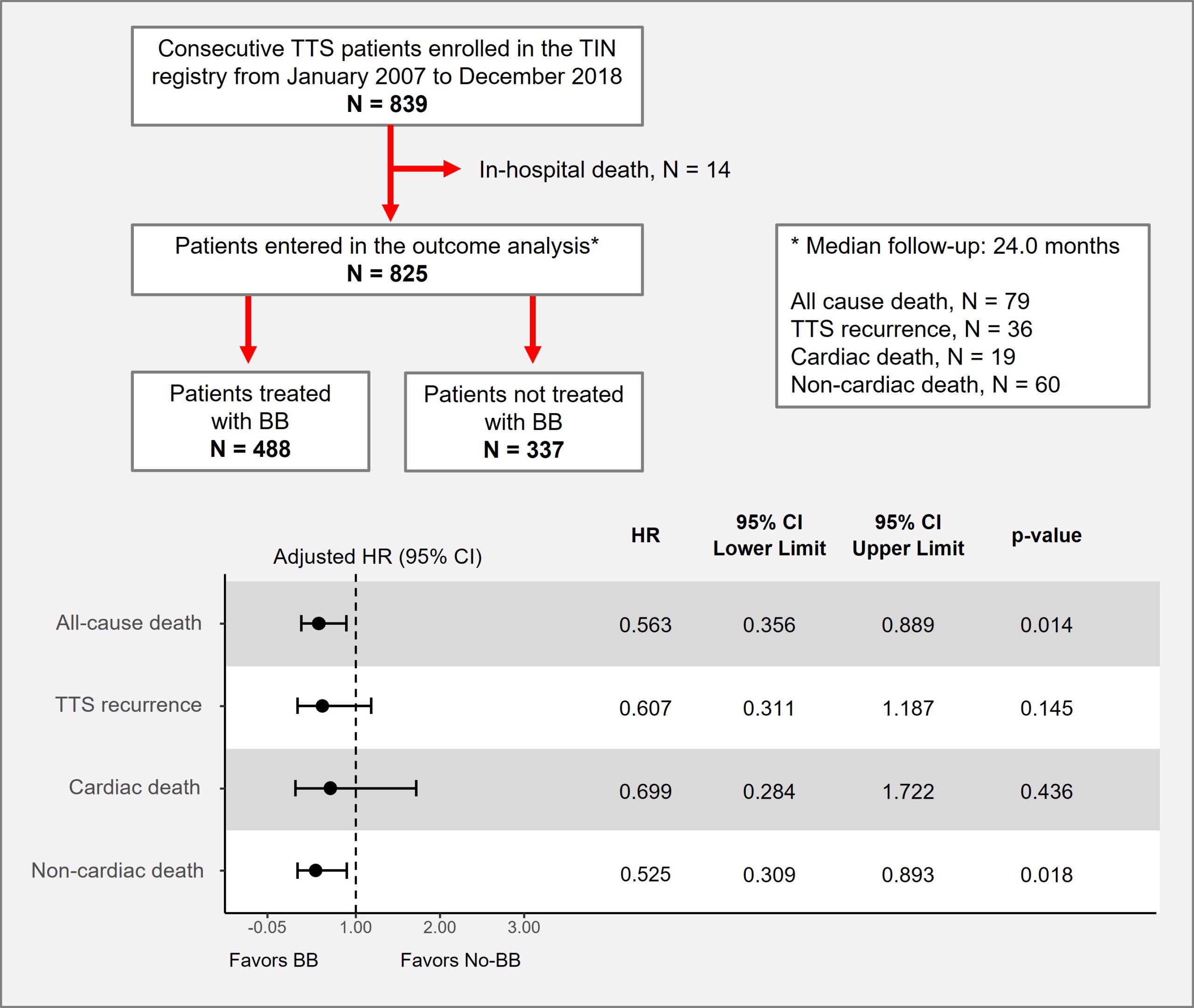
The median follow-up time was 24 months. The Kaplan-Meier analysis showed a significantly higher survival free from all-cause death (Log-Rank=0.004) and from non-cardiac death (Log-Rank=0.006) in patients treated with beta-blockers (Figure 1). Survival free from TTS recurrence and from cardiac death was not statistically different between groups.
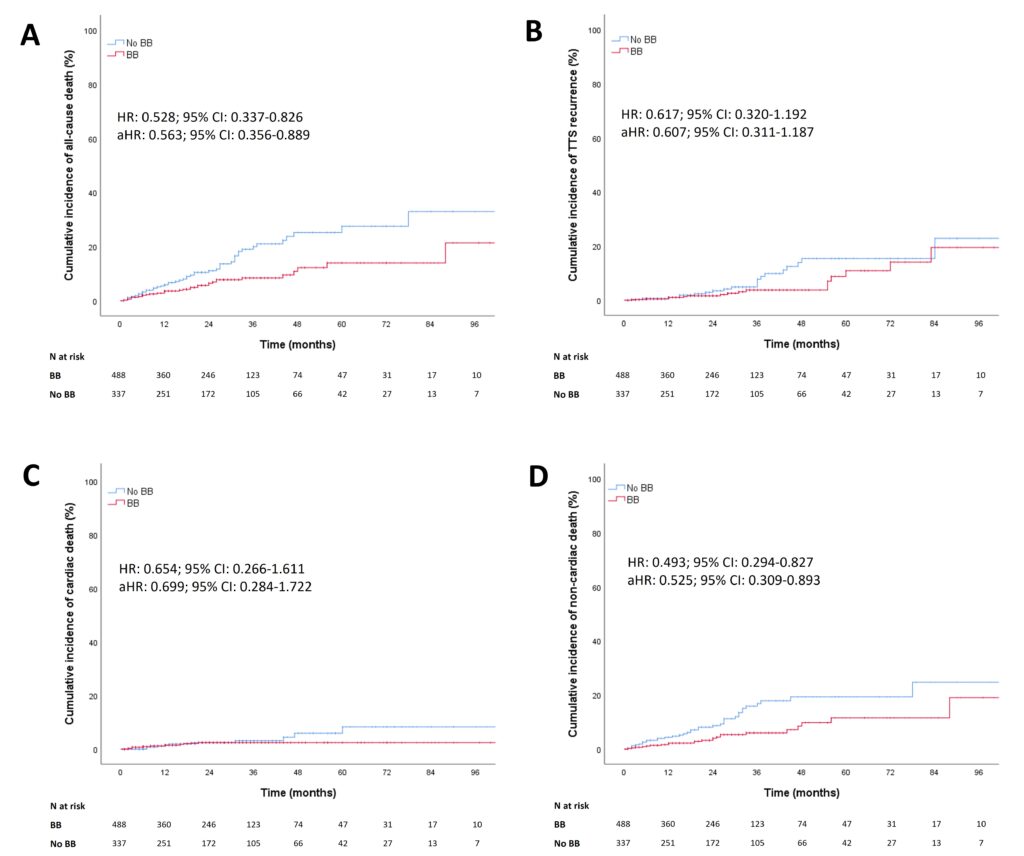
The propensity score–weighted adjusted regression analysis confirmed the significantly lower risk of all-cause death (adjusted HR:0.56; 95%CI:0.36-0.89) and non-cardiac death (adjusted HR:0.56; 95%CI:0.31-0.89) in patients treated vs. those not treated with beta-blockers, and no difference for TTS recurrence and cardiac death between groups (Figure 2).
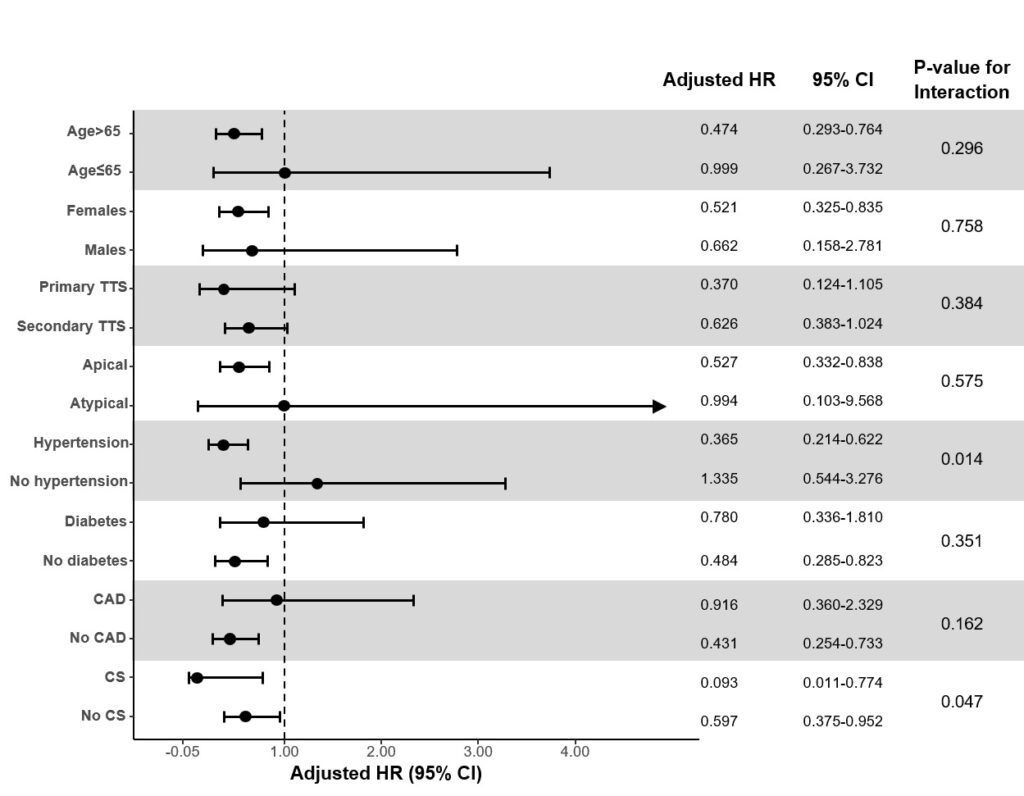
The effect of beta-blocker treatment on all-cause mortality was consistent among the prespecified subgroups of interest except for hypertension and cardiogenic shock (Figure 3). The survival effect of beta-blockers was higher in patients with hypertension, with a significant subgroup interaction (pinteraction=0.014). The survival benefit of beta-blockers was also higher among patients who developed cardiogenic shock during the acute phase than in those who did not (pinteraction=0.047).
DISCUSSION AND CONCLUSIONS
The TTS pathophysiology seems to reflects the cardiovascular response to sudden raise in serum catecholamine concentrations, often in the context of acute emotional or physical stressful events.[3] In patients recovering and being discharged after the index event, long-term treatment with beta-blockers might reduce the sympathetic overdrive and the risk of adverse events at long term.
The main findings of this real-world multicenter study can be summarized as follows:
i) Beta-blockers were prescribed in about 60% of TTS patients at discharge;
ii) Beta-blocker treatment was associated with lower risk of overall mortality at long-term follow-up;
iii) the beneficial effect of beta-blockers on overall survival was significantly higher in patients with hypertension and in those who developed cardiogenic shock during the acute phase.
This observational study reports in a large multicenter real-world population the association of beta-blocker treatment with higher survival and identified specific categories of patients where the use of beta-blockers appears particularly advantageous, such as in TTS patients with hypertension and in those who developed cardiogenic shock during the acute phase.
Although needing confirmation by randomized clinical studies, these findings could have important implications for a more rationale use of beta-blockers in the long-term management of TTS patients.
REFERENCES
1 Redfors B, Vedad R, Angerås O, et al. Mortality in takotsubo syndrome is similar to mortality in myocardial infarction – A report from the SWEDEHEART registry. Int J Cardiol 2015;185:282-9.
2 Templin C, Ghadri JR, Diekmann J, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. The New England journal of medicine 2015;373:929-38.
3 Akashi YJ, Nef HM, Lyon AR. Epidemiology and pathophysiology of Takotsubo syndrome. Nature reviews Cardiology 2015;12:387-97.
4 Borchert T, Hübscher D, Guessoum CI, et al. Catecholamine-Dependent β-Adrenergic Signaling in a Pluripotent Stem Cell Model of Takotsubo Cardiomyopathy. Journal of the American College of Cardiology 2017;70:975-91.
5 Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. The New England journal of medicine 2005;352:539-48.
6 Santoro F, Ieva R, Musaico F, et al. Lack of efficacy of drug therapy in preventing takotsubo cardiomyopathy recurrence: a meta-analysis. Clin Cardiol 2014;37:434-9.
7 Isogai T, Matsui H, Tanaka H, et al. Early β-blocker use and in-hospital mortality in patients with Takotsubo cardiomyopathy. Heart (British Cardiac Society) 2016;102:1029-35.
FIGURE LEGENDS
Figure 1. Kaplan-Meier curves for survival free from all-cause death (A), TTS recurrence (B), cardiac death (C), and non-cardiac death (D) in patients treated or not with beta-blockers at long-term follow-up.
aHR, adjusted hazard ratio; BB, beta-blockers; CI, confidence interval; HR, hazard ratio; TTS, takotsubo syndrome.
Figure 2. Study selection process and adjusted Cox regression analysis.
aHR, adjusted hazard ratio; BB, beta-blockers; CI, confidence interval; HR, hazard ratio; TIN, Takotsubo Italian Network; TTS, takotsubo syndrome.
Figure 3. Subgroup analysis for the risk of the primary outcome in patients treated or not with beta-blockers.
BB, beta-blockers; CAD, coronary artery disease; CI, confidence interval; CS, cardiogenic shock; HR, hazard ratio, TTS, takotsubo syndrome.
aHR, adjusted hazard ratio; BB, beta-blockers; CI, confidence interval; HR, hazard ratio; TTS, takotsubo syndrome.
The p-value expresses the statistical heterogeneity of the beta-blocker treatment effectiveness between the subgroups of interest.



Related Posts